A 80 year old male came with chief complaints of fever, vomiting, decrease urine output since 2 days
- Get link
- X
- Other Apps
A 80year old male came with Fever,Vomiting, decreased urine output
K.ROHITH DHARMA , 9thsemester
HALLTICKET NO - 1701006074
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
CASE PRESENTATION:
A 80yr old male, resident of marrigudam, farmer by occupation presented to our opd on 31st may 2022 with
CHEIF COMPLAINTS
C/O Fever since 3days
C/O decreased urine output since 2days
C/O vomiting 2days back
HISTORY OF PRESENT ILLNESS:
- Patient was apparently asymptomatic 10yrs back then he developed fever associated with chills insidious in onset ,gradually progressive with no diurnal variations and relieved on medication and also decreased urine output , burning micturition is present then he went to a hospital there he was told as renal failure(AKI) and 2sessions of dialysis was done.
From then he was on medication with diuretics(Tab.Furosemide) as he was suffering from oliguria.
- Later he developed recurrent episodes of fever associated with chills and also burning micturition which was relieved by tablets given by local hospital.
- Now 8days ago he developed
FEVER insidious in onset ,gradually progressive with no diurnal variations and relieved on medication associated with chills and generalised body pains . It is not associated with cough ,cold and night sweats.
Decreased urine output and there is burning micturition which is experienced at the start of urinary flow and relieved after urination and is not associated with any hematuria.
H/o vomiting of 1episode 7days ago with food particles as content and non bilious and non foul smelling.
Later sob since 6days which is of insidious in onset,gradually progressive, of grade 3 (NYHA)developed associated with wheezing,pedal edema.
no orthopnea,no paroxysmal nocturnal dysuria
- No h/o facial puffiness
- No H/O loin pain
PAST HISTORY
K/c/o HTN since 24years and is on regular treatment of Tab.Telmisartan 40mg
NO DM,ASTHMA,CAD
Nephrectomy was done 27yrs ago donated left kidney to his brother.
PERSONAL HISTORY
Marital status - married
Occupation - Farmer
Appetite - Decreased
Diet - Mixed
Bowel and bladder movements - decreased and oliguria associated with burning micturition and feeling of incomplete voiding.
Addictions - he was occasional alcoholic and smoker 27 years back smokes daily 2-4 beedis per day. And after nephrectomy was done he quit smoking.
FAMILY HISTORY
No significant
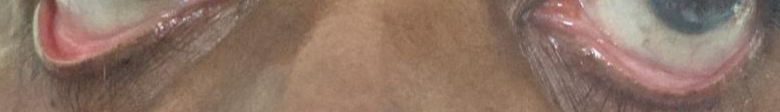
GENERAL EXAMINATION :
Patient is conscious , coherent, cooperative and well oriented to time ,place ,person.
moderately built and nourished.
Pallor present
pedal edema present ,pitting type
No icterus , cyanosis , lymphadenopathy
VITALS
Temp:Febrile
BP : 140/ 90mm Hg(on medication)measured in supine position in both arms .
PR : 86/ Min normal voulme ,regular rhythm,normal character ,no radiofemoral delay,radioradial delay.
RR : 18/ Min
SPO2: 97% on RA
GRBS:106mg/dl
SYSTEMIC EXAMINATION
CARDIO VASCULAR SYSTEM :
- Elliptical and bilateral symmetrical chest
- No visible pulsations,engorged veins,scars,sinuses on the chest wall.
- No raised JVP.
- Apex beat palpable at 5th intercostal space medial to midclavicular line .
- S1, S2 heard.
- No murmurs.
RESPIRATORY SYSTEM: for
- Shape of chest is elliptical and b/l symmetrical
- Trachea appears to be central
- Expansion of chest equal on both sides
- BAE + , diffuse wheeze+
- Vesicular breath sounds heard.
PER ABDOMEN :
- No abdominal distention, visible pulsations,engorged veins,scars,sinuses.
- soft , nontender ,no organomegaly.
- Bowel sounds present.
CNS :
- Higher mental functions intact.
- No signs of meningeal irritation.
- Sensory system :Normal
- Motor System :Normal
- Cranial nerves :Intact
- Reflexes: Right. Left.
Biceps. ++. ++
Triceps. ++. ++
Supinator ++. ++
Knee. ++. ++
Ankle ++. ++
- Gait: normal
Clinical pictures:
Serum electrolytes:
RFT:
On 31/05
Serum creatinine:9.1mg/dl
Blood urea:164mg/dl
On 1/06
Urea - 129mg/dl
ECG
USG
- Raised echogenicity of right kidney
- Normal size of kidney
- Mild hydronephrosis
- Not visible left kidney
Urine culture and sensitivity:
Provisional diagnosis -
AKI (2° to urosepsis) on CKD might be due to recurrent urinary tract infection.
TREATMENT:
1.INJ.LASIX 40 mg IV/BD
2.INJ PIPTAZ 4.5gm IV/STAT
3.INJ.PANTOP 40 mg IV/OD
4.INJ ZOFER 4 MG IV/SOS
5.INJ NEOMOL 100ml/IV/SOS
6.NEB.BUDECORT 12 HRLY
DUOLIN 6 HRLY
7.TAB. DOLO 650mg/TID
8.CREMAFFIN syrup 15ml PO/SOS
9.STRICT I/O CHARTING
10.BP,TEMPERATURE MONITORING 4 HRLY
- Get link
- X
- Other Apps



























Comments
Post a Comment